Rhinoplasty, also known as aesthetic nasal reconstruction or “nose job” to the general public is a plastic surgery procedure done to correct the size and shape of the nose. Plastic surgery of the nose has its roots in ancient Egyptian medical literature dating back to almost 3000BC. The first modern rhinoplasty procedure is often credited to American John Orlando Roe, an otolaryngologist/ENT surgeon who published his technique in 1887. Since then with the advent of improved medical technology and instrumentation rhinoplasty has evolved to become one of the most common but yet the most difficult procedure in plastic surgery. Successful rhinoplasty results require a surgeon who is extremely knowledgable about both the anatomy and function of the nose. The surgeon must be meticulous, have an artistic eye and always strive for perfection. The objective of rhinoplasty is not just about making the nose look better but also to breathe better. With Dr Scaccia’s dual/double board certification in Facial Plastic Surgery and Otolaryngology (Ear,Nose, and Throat/ENT), he is ideally trained to perform rhinoplasty.
Dr Scaccia is also the recipient of the Jack Anderson Award (Dr Anderson is one of the early pioneers in rhinoplasty) for having the highest score in the U.S. in the Facial Plastic Board certifying exam. He has performed countless rhinoplasties since 1990. Dr Scaccia wrote one of the first book chapters in the world on how to perform rhinoplasty and endoscopic sinus surgery at the same time. Revision or redo rhinoplasty is even more technically demanding and Dr Scaccia often performs revisions/corrections of rhinoplasty surgery that patients had elsewhere that resulted in complications. Although complications or results less than perfect can happen to any surgeon these events are rare at Riverside as Dr Scaccia strives for excellent results every time he operates. Often only one rhinoplasty will be performed in one day so that his entire attention will be devoted to that patient.
Depending on the needs of a particular patient Dr Scaccia is capable of performing either totally closed/endonasal or scarless rhinoplasty or if necessary an open rhinoplasty with a hidden/external incision. With his gentle technique and meticulous surgery swelling is often minimal and many patients are often able to return to work in a week. Special dressings are placed in the nose at the time of surgery that allows the patient to breathe through their nose as soon as they awake from anesthesia and during the entire recovery period.
Dr Scaccia’s philosophy is that since every person’s face is unique so should be the nose that is reconstructed. In the preoperative office discussions Dr Scaccia will listen to your concerns and will perform an extensive internal nasal fiberoptic exam and external review of your nose. Many pictures of you from several angles along with smiling and at rest will be taken and reviewed so that both the surgeon and patient are in agreement over your expected result. The desired final result utilizing laser printing imaging will presented to you for your approval. The surgery is performed with you completely asleep under general anesthesia by one of Riverside’s board certified physician anesthesiologists. Utilizing Dr Scaccia’s skills and experience along with the highly qualified and caring staff at his Joint Commission accredited Riverside Surgery Center everything will be done to make sure your rhinoplasty experience is pleasant and successful.
View Rhinoplasty before/after pictures in our photo gallery.
Surgery of the Nose
Every year, half a million people who are interested in improving the appearance of their noses seek consultation with facial plastic surgeons.
Some are unhappy with the noses they were born with, and some with the way aging has changed their nose. For others, an injury may have distorted the nose, or the goal may be improved breathing. But one thing is clear: nothing has a greater impact on how a person looks than the size and shape of the nose. Because the nose is the most defining characteristic of the face, a slight alteration can greatly improve one’s appearance.
If you have wondered how nose surgery, or rhinoplasty, could improve your looks, self-confidence, or health, you need to know how rhinoplasty is performed and what you can expect.
Successful facial plastic surgery is a result of good rapport between patient and surgeon. Trust, based on realistic expectations and exacting medical expertise, develops in the consulting stages before surgery. Your surgeon can answer specific questions about your specific needs.
Is Rhinoplasty for You?
As with all facial plastic surgery, good health and realistic expectations are prerequisites. Understanding nasal surgery is also critical. Since there is no ideal in rhinoplasty, the goal is to improve the nose aesthetically, making it harmonize better with other facial features.
Skin type, ethnic background, and age are important factors to be considered in discussions with your surgeon prior to surgery. Before the nose is altered, a young patient must reach full growth, usually around age fifteen or sixteen. Exceptions are cases in which breathing is severely impaired.
Before deciding on rhinoplasty, ask your facial plastic surgeon if any additional surgery might be recommended to enhance the appearance of your face. Many patients have chin augmentation in conjunction with rhinoplasty to create a better balance of features.
Making the Decision for Rhinoplasty
Whether the surgery is desired for functional or cosmetic reasons, your choice of a qualified facial plastic surgeon is of paramount importance. Many facial plastic surgeons are trained in both ear, nose, throat, and facial cosmetic surgery, which provides you, the patient, with the highest level of training and expertise. Your surgeon will examine the structure of your nose, both externally and internally, to evaluate what you can expect from rhinoplasty. You are most likely to be pleased with the results of your surgery if you have a realistic idea of what nasal surgery can and cannot do.
You can expect a thorough explanation of the surgeon’s expectations and the risks involved in surgery. Following a joint decision by you and your surgeon to proceed with rhinoplasty, the surgeon will take photographs of you and discuss the options available. Your surgeon will explain how the nasal structures, including bone and cartilage, can be sculpted to reshape the nose and indicate how reshaping the chin, for example, could enhance the desired results.
After conducting a thorough medical history, your surgeon will offer information regarding anesthesia, the surgical facility to be used, and the costs for the procedure.
Understanding the Surgery
The definition of rhinoplasty is, literally, shaping the nose. First, incisions are made and the bone and cartilage support system of the nose is accessed. The majority of incisions are made inside the nose, where they are invisible. In some cases, an incision is made in the area of skin separating the nostrils. Next, certain amounts of underlying bone and cartilage are removed, added to, or rearranged to provide a newly shaped structure. For example, when the tip of the nose is too large, the surgeon can sculpt the cartilage in this area to reduce it in size. The angle of the nose in relation to the upper lip can be altered for a more youthful look or to correct a distortion.
The tissues are then redraped over the new frame and the incisions are closed. A splint is applied to the outside of the nose to help retain the new shape while the nose heals. Soft, absorbent material may be used inside the nose to maintain stability along the dividing wall of the air passages called the septum. Alternatively, soft nasal supports that permit nasal breathing post-operatively can be placed.
What to Expect After the Surgery
Immediately after surgery, a small splint will be placed on your nose to protect it and to keep the structure stable for at least five to eight days. If packing is placed inside the nose during surgery, it is removed the morning following the surgery. Your face will feel puffy,especially the first day after surgery. Pain medication may be required. Your surgeon will advise you to avoid blowing your nose for seven days after surgery. In the immediate days following surgery, you may experience bruising and minor swelling in the eye area. Cold compresses often reduce the bruising and discomfort. Absorbable sutures are usually used that do not have to be removed. Nasal dressing and splints are usually removed six or seven days after surgery.
It is crucial that you follow your surgeon’s directions, especially instructions to keep your head elevated for a certain period after surgery. Some activities will be prohibited in the weeks after the procedure. Sun exposure, exertion, and risk of injury must be avoided. If you wear glasses, special arrangements must be made to ensure that the glasses do not rest on the bridge of the nose. Tape and other devices are sometimes used to permit wearing glasses without stressing the area where surgery was performed.
Follow-up care is vital for this procedure to monitor healing. Obviously, anything unusual should be reported to your surgeon immediately. It is essential that you keep your follow-up appointments with your surgeon.
Insurance does not generally cover surgery that is purely for cosmetic reasons. Surgery to correct or improve nasal function or surgery for major deformity or injury may be reimbursable in whole or in part. It is the patient’s responsibility to check with the insurance carrier for information on the degree of coverage.
Frank Scaccia, MD, David Stepnick, MD, Anthony Maniglia, MD
Since its introduction in the United States by Kennedy in 1985, functional endoscopic sinus surgery (FESS) has gained widespread acceptances and popularity and has achieved success in treating inflammatory sinus disease.1Although complications have been reported, the procedure, when performed properly in trained hands, is usually not only efficacious but also safe.2-5 Because FESS is an endonasal approach, it avoids external incisions and possible cosmetic problems. Because chronic sinusitis is a very common health problem affecting up to 40 million people each year in the United States, the demands for this surgery will probably continue to grow.
Rhinoplasty is another surgical procedure that has enjoyed increased public interest as members of our society become more conscious of their personal health, their appearance, and the ability to make changes therein. One survey indicated that up to 40% of all adults in United States are not happy with the external shape of their nose. Like sinus surgery, rhinoplasty is very safe, and its results are satisfying to surgeon and patients alike.
Combining septoplasty or turbinate reduction with rhinoplasty has been done for many years and seems to be a logical outcome of procedures performed on a defined anatomic subsite that can achieve cosmetic enhancement while simultaneously improving the nasal airway. With the advent of endonasal sinus surgery, rhinoplasty candidates who also suffer from chronic nasal and/or sinus ailment such as sinusitis, sinus headache, post nasal drip and congestion can have these conditions addressed during the same operation. Similarly, patents who are candidates for FESS often desire cosmetic improvement of the external nose and are willing to undergo the cosmetic portion of the procedure during the same operation, whereas they may be reluctant to undergo for surgery for cosmetic reasons only. The advantages of concurrent surgery are multiple and include the need for only one general anesthetic, less total time needed for recovery (and thereby a shorter absence from work or school), and overall lower medical costs than if the two procedures were performed separately.
This chapter discusses the work-up and preparations needed to perform combined rhinoplasty and sinus surgery procedures, the requirement for a safe surgical approach that will help to ensure a success outcome, postoperative care recommendations, a review of the current literature, the advantages and disadvantages of performing these procedures at the same surgical settings, and an evaluation of our personal results.
Preoperative Evaluation
Virtually all patients who are candidates for simultaneous rhinoplasty and FESS seek the advice and treatment of a physician because of their sinus complaints. As with any presenting problem, the clinician should elicit a through medical history with a particular focus on the sinus complaints as well as any functional and nasal deformities. Aspects that should be addressed include the duration of symptoms, associated allergic symptoms, overuse of topical decongestants, prior nasal surgery, failure to respond to medical therapies in the past, and trauma. In addition, if headaches and facial pressure are described, their exact location and possible association with certain allergic factor and visual disturbances should be ascertained. Migraines or neuralgias should be considered in the differential diagnosis.
Patients who are initially seen by the physician for a cosmetic consultation also need a complete history and physical examination. Occasionally, chronic nasal or sinus problems are diagnosed that require surgery because medical management has failed. These patients may very well welcome the opportunity to have both of their problems handled during the same surgical procedure.
Anterior rhinoplasty is performed both to and after decongestion of the nose with 1% Neo-Synephrine to obtain a more accurate assessment of the turbinates’ role in nasal obstruction. Following this, a topical anesthetic such as 4% lidocaine is sprayed on pledgets placed in the nasal cavity, so that a small fiberoptic nasal endoscope can be passed painlessly, allowing a more thorough examination of the internal nose. Many surgeons connect the fiberoptic endoscope to a camera or monitor system so that both the patient and possibly the family members can visualize the nasal anatomy during the examination. In addition, preoperative nasal cavity pictures can be taken with this system, allowing documentation in the chart and better communication with the referring physician. Using the fiberoptic scopes, posterior septal spurs and deviations, inferior turbinate pathologies, purulent secretions, polypoid or polyp formation, adenoid hypertrophy, and obstruction of the osteomeatal outflow tract can be identified.
Once the endonasal examination is completed, attention can be directed to the aesthetic assessment of the nose. This is done systematically beginning at the nasofrontal angel and ending at the nasolabial angle. Note is also made of the overall profile, including such elements as the position of the forehead and chin. Spreader grafts for a narrowed nasal valve and/or a strut for a poorly supported tip are at times deemed functionally necessary based on the examination, and their outward effect on the appearance of the nose should be discussed. In addition, the need for an external transcolumeller incision should be discussed with the patient if its need is anticipated. Finally, standard multiple-view photographs of the patient are taken for both medical and legal purposes and enlargement. Some surgeons use computer imaging system to help explain to their patient how the proposed surgery will affect their appearance. In our experience however, this often results in unrealistic patient expectations, which may lead to possible dissatisfaction. For enlargements, we use 6 X 9 inch color copies made from our original slides, which can be viewed directly or flipped over and transilluminated on an x-ray view box. This allows the surgeon to trace the preoperative patient profile with a pencil and then to draw the anticipated profile on the contralateral view to show the patient in a very basic and understandable way what the likely postoperative result will be.
After a thorough history and physical examination have been completed, there are still a few more important steps that must be taken before a final decision is made about the need for surgery. Sinus surgery, except in emergency situations, should almost never be offered to the patient unless aggressive medical treatment has been attempted in the past and has failed. Such medical therapy may include long -term antibiotic directed at the most likely sinusitis causing pathogens, oral decongestants, topical steroid preparations, and allergic desensitization therapy, if indicated. If these approaches have failed and rhinoscopic examination demonstrates an obvious anatomic derangement or pathology that could account for the patient’s symptoms, a complete coronal CT scan without contrast of the paranasal sinuses is ordered. The completed CT scan is reviewed with the patient, noting any functional deformity or disease that may explain the condition and may be amenable to surgical management.
Surgical Technique
Once the need for surgery has been established, certain preoperative steps should be followed. Obviously, the possible risks and benefits of both of the endoscopic sinus surgery and the rhinoplasty portion of the procedure must be discussed. A detailed explanation of these important issues may be supplemented by other educational materials such as a detailed handout, booklet, or videotape. The patient is informed that the functional (sinus) part of the operation will be performed first and, if for any reason an intraoperative problem occurs that might interfere with further surgery, the cosmetic portion will be abandoned or possibly performed at a later date. He or she is also informed that all aspirin containing products, nonsteroidal anti-inflammatory agents, and vitamin E must be stopped at least 2 weeks prior to the date of surgery because excessive intraoperative bleeding is often a cause of lack of completion of the sinus procedure as well as potential morbidity. Some physicians routinely use perioperative corticosteroid and antibiotic therapy in all patients unless these are contraindicated.
At the time of surgery, intravenous antibiotics and steroids may be initiated on call to operating room. Although deep sedation may be used, general anesthesia is preferred for these combined cases. Hypotensive general anesthesia (systolic 80 to 90 mmHg) may be used to minimize bleeding. A moist throat pack is placed in the oropharynx to collect any bloody runoff and to avoid swallowing of blood during anesthesia, which may cause discomfort and vomiting postoperatively. All CT films and preoperative pictures are displayed in an easily accessible area of the operating room suite. Cocainized 3-inch Cottonoid pledgets are placed in the right and left nasal cavities prior to the skin preparation to maximize internal nasal vasoconstriction. Sinus surgery and septoplasty, if needed, are always addressed first, since bleeding and swelling from the rhinoplasty would make endoscopic visualization difficult. All resected septal cartilage, bone, and turbinate tissue are preserved in saline solution until the completion of the procedure so that grafts may be readily available if they are needed later.
The sinus surgery is performed with both the 4.0 -mm, 0- degree and 25-degree wide-angle rigid endoscope utilizing a video monitor to minimize surgeon discomfort resulting from bending over during the procedure. This setup is helpful in a teaching setting. Well-placed injections of 1% lidocaine with 1:100,000 epinephrine at the uncinate process and middle turbinate edge are critical for achieving operative hemostasis. In addition, frequent blotting with topical 1:1000 adrenaline in the ethmoid cavity also minimizes oozing. The basic endoscopic technique utilized by the authors is that described by Messerklinger and others, which has been presented extensively elsewhere.8 Complete resection of the uncinate process and associated diseased agger nasi cells is imperative to maximize the chances of success and deserves special note.
Often septoplasty must be performed prior to enthmoidectomy in patients with severe deflection so that comfortable access and visualization can be obtained during the surgical procedure. Rarely, partial resection of the septum is necessary in the area of sinus obstruction, and this can be accomplished via an incision made posteriorly using the endoscope and sickle knife. When inferior turbinate reduction is performed, either directly by resection or by tissue ablation with KTP laser, cautery, or cryosurgery, it is always performed after the sinus procedure because bleeding and/or swelling can occur, thereby obscuring the field.
A complete anterior and posterior ethmoidectomy is performed in almost all cases except those in which only limited osteomeatal diseases has been identified on CT. Often disease is found in the posterior ethomid and frontal recess region, even if this is not clearly demonstrated on preoperative radiographs. There are several advantages to performing a total ethmoidectomy. These include a more thorough exenteration of diseased sinus tissue, easier inspection and assessment of the cavity during the postoperative period, less bleeding intraoperatively and postoperatively when all diseased sinus tissues have been removed, and easier placement of postoperative splints for middle turbinate stabilization. The added operative time and additional risk in performing a total versus partial ethmoidectomy should be minimal in experienced hands.
One of the most discussed and perhaps controversial issues in FESS is the management of the middle turbinate. Postoperative lateralization of a preserved middle turbinate is often cited as the most frequent cause of postoperative failure. The middle turbinate becomes even more of a concern when concurrent rhinoplasty and lateral osteotomies are included as part of the procedure. A floppy middle turbinate in this situation may be even more prone to lateralize and obstruct a newly created osteomeatal outflow tract.
Earlier attempts in our series to prevent this complication by partially resecting the middle turbinate (when combining rhinoplasty and sinus procedures) were successful but appeared to cause a prolonged period of healing of the ethmoid cavity. Edema and granulation tissue were noted to persist up to 3 months postoperatively in some patients. More recently, every effort has been made to preserve the middle turbinate at least partially utilizing the Boomerang middle turbinate glove (Xomed Surgical Products, Jacksonville, FL) to prevent lateralization (Fig. 24-1). Earlier use of an expandable Merocel sponge (Xomed Surgical Products, Jacksonville, FL) for this purposes has been abandoned because it resulted in increased tissue reaction. In our hands, use of the middle turbinate glove appears to be associated with a significant decrease in postoperative edema with almost complete healing of the ethmoid cavity by 3 to 4 weeks. In addition, no middle turbinate lateralization or drift has occurred in these 13 consecutive cases. These splints are now used by us in all cases after lateral resections for concha bullosa. When one or both middle turbinates are resected for hypertrophic enlargement, absorbable gelatin film packs are placed lateral to cut middle turbinates remnants. Both the middle turbinates gloves and absorbable gelatin film, when needed, are placed during the procedure prior to performing rhinoplasty and are left undisturbed for up to 2 weeks postoperatively. Silastic nasal splints, placed bilaterally, minimize the possibility of postoperative scarring.
Rhinoplasty is begun only after endoscopic sinus surgery, septoplasty and/or turbinate reduction have been completed. The cavities are inspected for persistent bleeding, which must be controlled prior to proceeding with cosmetic portion of the operation. Surgicel is helpful in packing the nasal cavity temporarily during the steps of rhinoplasty. Additional surgery at this point, especially nasal osteotomies, should not be attempted if complications such as a cerebrospinal fluid (CSF) leak or orbital penetration with fat herniation occurred during the endoscopic sinus procedure. If FESS is uneventful, rhinoplasty can be initiated using the same technique that would be used if it were performed independently. Either an external or endonasal approach can be used. Nasal osteotomies should not be discouraged, assuming that endoscopic sinus surgery is uncompleted, if these are needed for nasal pyramid straightening or narrowing. No significant complications have been encountered in our hands; similar conclusions have been reached by others.
Tip manipulation and grafting are also carried out as necessary. Alloplastic augmentation, however, may be contraindicated if the concurrent sinus procedures were performed on an acutely infected sinus cavity containing purulent material. If infection is suspected preoperatively, antibiotics should be given to eradicate the acute infection. If it is encountered intraoperatively, one should consider abandoning the cosmetic portion of the procedure, especially if cartilage grafts or alloplastic implants are needed.
Alar base narrowing procedures can also be performed, although increased tenderness in this area during the initial postoperative period may restrict some of the postoperative care necessary for ethomoid cavity debridement. This discomfort usually resolves within the first few weeks and is usually not associated with significant problems. At the completion of the procedure, _ – inch Steri-Strips (Medical – Surgical Division/3M, St. Paul, MN) are applied to the nasal skin, an Aquaplast thermoplastic cast is placed externally, and bacitracin-coated Telfa packing (Kendall Healthcare Products, Mansfield, MA) is used for packing. Eight-centimeter long, 14-F tracheal suction catheters may be placed in each nasal cavity in the packing material to allow some postoperative airflow in an attempt to minimize patient discomfort.
Postoperative Care
Prophylactic antibiotics are prescribed for up to 2 or 3 weeks. In the first postoperative visit the packing is removed , and this is routinely scheduled on the second or third postoperative day. The patients are instructed to begin instilling Ponaris (Jamol Laboratories, Inc, Emerson, NJ) drops into each nasal cavity three times a day for lubrication. One to two weeks later the middle turbinate gloves or, if still present, the absorbable gelatin packs are removed from the nose, and direct endoscopic visualization and debridement of crust and thickness secretions is instituted on a weekly to biweekly basis until the ethmoid cavities are clean and healed. Daily saline nasal douching utilizing a Water Pik at home is also instituted at this time. Nasal saline pray is also helpful.
Care of the external nose is identical to that recommended if rhinoplasty were performed without concomitant sinus surgery. The Aquaplast thermoplastic splint is generally removed about 1 week postoperatively and Steri-Strips are replaced as necessary and left in place for up to 3 weeks in all.
Results
We reviewed 186 consecutive patient who underwent FESS by one of us (FJS) in conjunction with septoplasty, rhinoplasty, and /or turbinate procedures. Twenty-eight of these patients also underwent cosmetic rhinoplasty. Follow up ranged from 6 months to 2 _ years. Surveys seeking information about perceived postoperative symptomatic results were sent to all 186 patients. Forty-nine patients responded, for an overall response rate of 26 percent. Ninety six percent of all patients who responded were pleased that they had undergone sinus surgery and felt that it made a positive impact on their general health and well-being. A similar satisfaction rate was seen in that cohort of surgery respondents who underwent simultaneous rhinoplasty and sinus surgery. Revision surgery was not required in any of the 28 rhinoplasty patients. No cerebrospinal fluid leak or orbital invasion occurred in patients with planned rhinoplasty procedures, and as a result, no change was necessary in the procedures done on this patient.
One case of hemorrhage significant enough to require return to the operating room occurred. Bleeding was noted in the region of the sphenoplalatine artery, which was probably transected after a very posterior resection of the middle turbinate. This was easily controlled with suction cautery and subsequent packing. We anticipate that this complication will become even less of a problem for us in the future because most middle turbinates are now being preserved. The experience of the other authors (AJM, DWS) in an additional 11 cases revealed no minor or major complications.
Two cases of simultaneous rhinoplasty and sinus surgery are now included to illustrate details of patient management and outcome.
Case Reports
Case 1
A 56 year old female presented with a history of chronic sinusitis and nasal obstruction. Despite prior aggressive medical treatment with long term antibiotics, decongestants, and topical nasal steroid therapy, she continued to complain of frontal headaches, postnasal drip and difficulty in breathing. In addition, she was also unhappy about the appearance of her nose and desired aesthetic improvement. Anterior nasal rhinoplasty demonstrated a deviated nasal septum that partially obstructed the right nasal cavity, enlarged inferior and middle turbinates, and inflammation of the sinus mucosa within the middle meatus bilaterally. External examination of the nose demonstrated a rather naked bony cartilaginous nasal hump and a wide bulbous tip. The patient was also made aware of her moderately recessed shin, which amplified her nasal deformity. A CT scan of the sinuses confirmed the presence of enlarged inferior turbinates and devited septum. In addition, there was also evidence of mild ethmoiditis and bilateral cancha bullosa with narrowing of each of the osteomeatal complexes. Because of these radiographic figures, in conjunction with her history and physical examination and her desire for simultaneous aesthetic improvement, a combined functional endoscopic sinus procedure and aesthetic rhinoplasty was offered and subsequently performed. In addition, an intraoral chin implant was placed to help improve the harmony of the facial profile, KTP laser ablation was performed on the inferior turbinates , and sharp dissection to remove the middle turbinate was used, preserving the medial wall on each side. As depicted in the postoperative pictures, a much more widely patent nasal sinus cavity has been created along with a more pleasing nasal and facial contour (Figs 24-3 to 24-5). At 1.5 years follow up the patient has had total relief from headache and postnasal drip and reports very significant improvement in nasal function. In addition, she was very satisfied with the appearance of her chin and nose.
Case 2
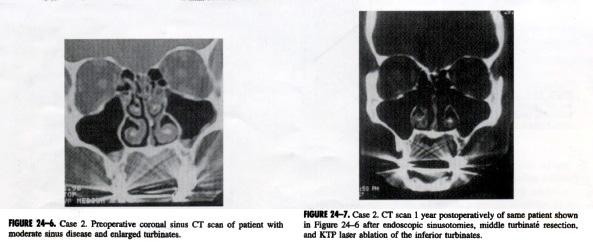
A 47-year-old female with a history of a prior reconstructive rhinoplasty 20 years earlier presented with chronic sinusitis and nasal obstruction. Maximal medical therapy with multiple antibiotics, decongestants, and steroids were tried over several years but produced little relief from headaches and nasal congestion. The patient was also not satisfied with the cosmetic result of her prior rhinoplsty. Intranasal examination demonstrated a deviated nasal septum to the left, swollen inferior turbinates, and a very inflamed sinus mucosa.
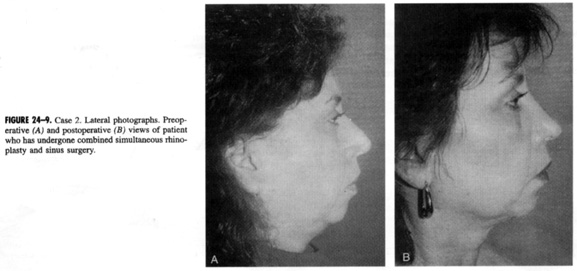
External nasal examination demonstrated an irregular nasal dorsum with a mild pollybeak formation. The tip cartilages were also grossly asymmetrical with a right-sided bossa protuberance and bilateral alar pinching that probably resulted from overzealous cartilage resection in the past. The alar pinching was thought to contribute to the nasal obstruction, especially with the deep inspiration. A CT scan demonstrated moderate mucoperiosteal thickening of the ethmoid, maxillary, and frontal sinuses with occlusion of the osteomeatal complexes. (Fig. 24-6). Because of the patient’s functional complaints and findings and aesthetic desires, a combined endoscopic sinus surgery procedure and open septorhinoplasty was performed. A complete anterior and posterior ethmoidectomy with maxillary entoscopy was done bilaterally. In addition, bilateral middle turbinectomies were performed to prevent postoperative lateralization. An external rhinoplasty approach was used because this was a revision case involving placement of multiple cartilaginous grafts to the tip from both auricles and the remaining septum.
As can be seen in the postoperative (CT scan, the nasal and sinus cavities are now widely patent and free of sinus pathology (Fig. 24-7). In addition, the irregularities resulting from the prior rhinoplasty has been corrected (Fig. 24-8 and 24-9). The patient at 1-year follow-up has enjoyed almost total relief from her prior sinus symptoms and is very happy with the more natural appearance of her nose.
Discussion
Although it was uncertain who was first to perform simultaneous rhinoplasty and endoscopic sinus surgery, Sherman and Matarasso 10 are credited with the first published reports of combining these two procedures. Despite an increasing number of patients who are candidates for simultaneous rhinoplasty and endoscopic sinus surgery, a paucity of information on this topic appears in the literature. In fact, only three subsequent publications have provided information about this concept.
Toffel, in the first large series reported in the literature, performed simultaneous rhinoplasty and FESS in 122 of 698 cases (19%).11 He described the technique for each of the two procedures as well as the functional results of the 698 FESS procedures for those patients who were still being followed at 1 and 3 years. Three case reports illustrated the utility of performing these procedures together, but the advantages, disadvantages and techniques were not addressed.
Glicklich and Lauretano considered the problem of the whether it is safe to perform osteotomies, which are often necessary for a rhinoplasty, in the presence of endoscopic ethmoidectomies.9 In a study using 14 fresh-frozen cadaver heads, extensive ethomoidectomies including marsupialization of the frontal recess and agger nasi areas were followed by medical and lateral osteotomies. There were no major comminutions along the osteotomies, nor did the fractures extend into either the orbit or base of the skull, suggesting that combining the procedures does not jeopardize patient safety. Additionally, the enlarged maxillary ostia created by the sinus surgery was not altered by the osteotomies or by dorsal narrowing. In each case a relatively thick buttress of bone composed of the anterior lacrimal crest and the ascending process of the maxilla separated the ethmoid surgical cavity from the line of osteotomy. The author advise caution in patients who have undergone previous lacrimal surgery, in those with preexisting pathways into the orbit or skull base, and in those who are to undergo osteotomies by methods that do not preserve the triangular nasal buttress or double osteotomies. Furthermore, they suggest that CT scans should be considered in patients in whom a rhinoplasty is planned who have undergone previous sinus surgery to verify that an iatrogenic skull base or orbital dehiscence has not been created.
Further details about the safety of combining these two procedures are given in the most recent series published. Rizk and colleagues had only one minor complication, postoperative hemorrhage in a series of 40 patients.12 They like us and other authors, recommend completing the endoscopic sinus surgery before beginning the rhinoplasty.
Summary
In summary, the indications for performing these two procedures during the same surgical sessions are, in essence, the same as for the procedures individually: failure of medical management of sinus disease and the desire of the patient for aesthetic improvement of the nose. Absolute or relative contraindications include a variety of medical conditions(e.g. bleeding disorders (especially when cartilabe grafts or alloplasts are considered necessary for the rhinoplasty), poorly conrolled hypertension, diabetes mellitus, or an asthmatic patient with nasal polyposis), gross infection of the sinuses, and complications encountered during the endoscopic procedure (excessive bleeding, orbital presentation, or CSF leak). In a patient who maybe considered a very poor surgical risk, sinus surgery should be avoided if at all possible. On the other hand, if FESS is absolutely necessary, the procedure can be done with appropriate anesthesia consultation, but the cosmetic portion of the procedure should be avoided. The advantages of performing concurrent surgery are significant and include one anesthetic episode, less total recovery time, and overall lower medical costs than if the two procedures were each performed separately. Disadvantages are minimal and include a potential inability to assess orbital complications from FESS (since osteotomies result in ecchymosis), increased nasal tenderness as a result of the rhinoplasty, possibly compromising the surgeon’s ability to perform postoperative cleaning, and more swelling and discomfort than would be likely with either procedure alone. Our experience and the literature reports support the premise that FESS combined with cosmetic rhinoplasty can be safe procedure in selected patients and can lead to functional and cosmetic results that are satisfactory to patients and surgeons alike.
Interested in learning more? Please contact the staff at riverside facial plastic surgery and sinus center about scheduling an appointment.